ICAPs
What is an Intensive Comprehensive Aphasia Program (ICAP)?
Intensive comprehensive aphasia programs (ICAPs) are a relatively new service delivery model for stroke rehabilitation. The number of ICAPs across the country is increasing due to a desire to approach aphasia rehabilitation from a holistic and biopsychosocial foundation, while also implementing intensive therapy, which has been found to yield effective therapeutic outcomes. The overarching goal of an ICAP is to maximize communication potential and improve life participation. In short, ICAPs are multi-faceted and take into consideration the many aspects of communication needs faced by persons with aphasia and their family caregivers.
ICAPs provide a minimum of three hours of therapy per day for two weeks, with some programs providing as many as four to six hours a day over a period of four to five weeks. Daily therapy should include individual sessions, group sessions, computer or technology-based therapy, and patient and family education. Persons with aphasia and their family caregivers who are enrolled in an ICAP may receive as many as 120 hours of focused language therapy over the span of one month, whereas a person in a standard therapy model receives approximately 8 to 12 hours of therapy in the same time frame. While research of the ICAP model is in its infancy, initial efficacy studies indicate positive patient outcomes across a variety of impairment-based and psychosocial domains.
Who are ICAPs best suited for?
Recent research suggests that ICAPs are best suited for persons with aphasia who are at least one year post stroke (Babbitt et al., 2016). Participants should be medically stable and be able to maintain alertness and attention all day. In previous research, approximately 11% of persons with aphasia who enroll in ICAPs do not make gains, suggesting that the majority of people who do enroll in ICAPs make gains in language and psychosocial function. Gender, type of aphasia, and severity of aphasia do not appear to impact the success of treatment in an ICAP model.
What does the Big Sky Aphasia Program’s ICAP offer?
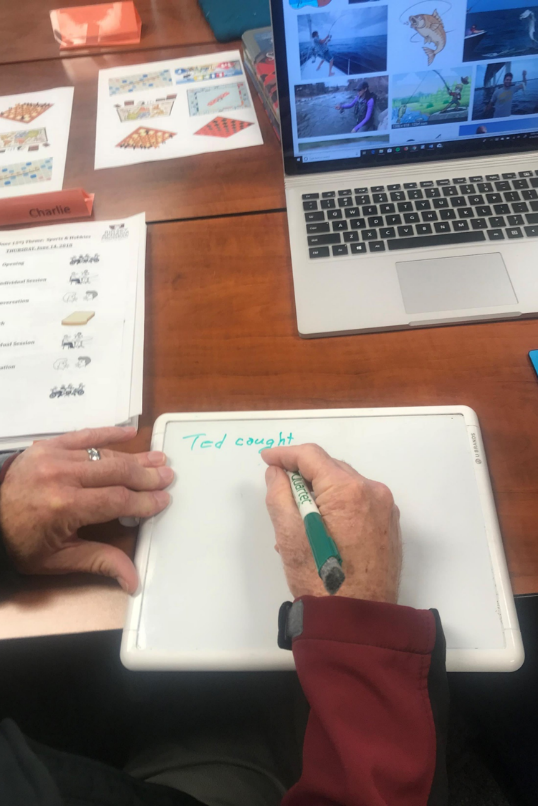
The Big Sky Aphasia Program’s ICAP at the University of Montana is designed with clearly defined intensity parameters, a concern for client, family caregiver, and clinician perspectives, and a focus on comprehensive therapy that addresses multiple modalities using strategies and recreational opportunities individualized to the person with aphasia and their family caregiver(s). The Big Sky Aphasia Program currently offers a summer ICAP for individuals with aphasia and/or apraxia of speech (and their family caregivers) who have had a stroke or acquired brain injury.

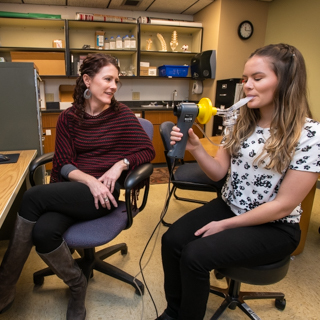
Our ICAP includes individual, small group, and technology-based therapy, as well as weekly caregiver education and caregiver group counseling. We also provide weekly recreational/community-based outings (e.g., adaptive fishing, aphasia-friendly art museum tours, aphasia-friendly movie-going) to support a Life Participation Approach to Aphasia. Participants receive speech and language therapy 4.5 hours per day, 4 days per week, for 3-4 weeks, depending on the specific ICAP program. Prior to beginning treatment, participants receive a comprehensive speech and language evaluation to determine their individual strengths and needs. The program culminates with post-treatment testing and a final family conference during the final week to discuss progress and to make recommendations for home programming and further services. The cost of the program fluctuates from session to session. Total costs include pre- and post-treatment assessment, all treatment and caregiver educational and counseling sessions, weekly recreational outings, and weekly hosted lunches.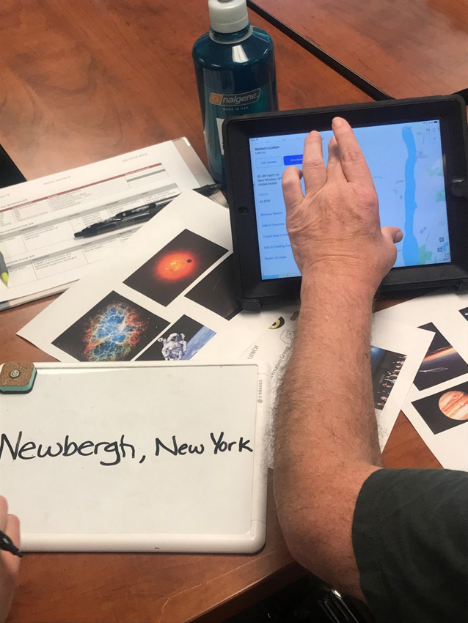
During the ICAP, we offer group caregiving counseling in collaboration with Dr. Kirsten Murray, who is a family counselor and Associate Professor at the University of Montana (Department of Counselor Education). We also have a phenomenal physical therapy department and clinic on campus, New Directions Wellness Center, and are happy to organize ongoing physical therapy or access to their accessible gym while you are attending our ICAP.
Published Research Articles about ICAPs
comprehensive aphasia program. Topics in Stroke Rehabilitation, 20(5), 398-408.
Babbitt, E., Worrall, L., & Cherney, L. R. (2015). Structure, processes, and retrospective
outcomes from an intensive comprehensive aphasia program. American Journal of
Speech-Language Pathology, 24(4), S854-S863.
Babbitt, E. M., Worrall, L., & Cherney, L. R. (2016). Who benefits from an intensive
comprehensive aphasia program? Topics in Language Disorders, 36(2), 168-184.
Baliki, M. N., Babbitt, E. M., & Cherney, L. R. (2018). Brain network topology influences
response to intensive comprehensive aphasia treatment. NeuroRehabilitation, 43(1), 63-76.
Escher, A. A., Amlani, A. M., Viani, A. M., & Berger, S. (2018). Occupational therapy in an
intensive comprehensive aphasia program: Performance and satisfaction outcomes. The
American Journal of Occupational Therapy, 72(3), 1-7.
Hoover, E. L., Caplan, D. N., Waters, G. S., & Carney, A. (2017). Communication quality of life
outcomes from an interprofessional intensive, comprehensive aphasia program (ICAP).
Topics in Stroke Rehabilitation, 24(2), 82-90.
Hoover, E. L., & Carney, A. (2014). Integrating the iPad into an Intensive Comprehensive Aphasia Program. Seminars in Speech and Language, 35(1), 25-37. doi:10.1055/s-0033-1362990
Hoover, E. L., & Carney, A. (2014). Integrating the iPad into an Intensive Comprehensive Aphasia
Program. Seminars in Speech and Language, 35(1), 25-37. doi:10.1055/s-0033-1362990
Off, C. A., Griffin, J. R., Murray, K. W., & Milman, L. (2019). Interprofessional caregiver
education, training, and wellness in the context of a cohort model for aphasia
rehabilitation. Topics in Language Disorders, 39(1), 5-28.
Persad, C., Wozniak, L., & Kostopoulos, E. (2013). Retrospective analysis of outcomes from two
intensive comprehensive aphasia programs. Topics in Stroke Rehabilitation, 20(5), 388-397.
Rodriguez, A., Worrall, L. E., Brown, K., Grohn, B., McKinnon, E., Pearson, C., . . . Copland, D. A.
(2013). Aphasia LIFT: Exploratory investigation of an intensive comprehensive aphasia
programme. Aphasiology, 27(11), 1339-1361.
Rose, M., Cherney, L. R., & Worrall, L. (2013). Intensive Comprehensive Aphasia Programs: An
international survey of practice. Topics in Stroke Rehabilitation, 3(20), 379-387.
Trebilcock, M., Worrall, L. E., Ryan, B., Shrubsole, K., Jagoe, C., Simmons-Mackie, N., . . . Le
Dorze, G. (2019). Increasing the intensity and comprehensiveness of aphasia services:
identification of key factors influencing implementation across six countries.
Aphasiology, 33(7), 865-887.
doi:http://dx.doi.org.weblib.lib.umt.edu:8080/10.1080/02687038.2019.1602860
Winans-Mitrik, R. L., Hula, W., Dickey, M. W., Schumacher, J. G., Swoyer, B., & Doyle, P. (2014).
Description of an Intensive Residential Aphasia Treatment Program: Rationale, Clinical
Processes, and Outcomes. American Journal of Speech- Language Pathology, 23, S330-
S342.