Identifying potential hospital bed shortages for people with disabilities
April 3, 2020
Recent models from ProPublica, Imperial College, and others predict that millions of people who contract COVID-19 will be hospitalized and many hospitals across the country may not be prepared to treat the influx of patients.
People with disabilities are particularly vulnerable to impacts from COVID-19, both directly and indirectly. While data about how this virus will impact the health and well-being of people with disabilities is currently limited, people with disabilities are often at greater risk of chronic health conditions, and thus may be more susceptible to infection. People with disabilities also face disruptions in services for daily needs, which could exacerbate conditions unrelated to COVID-19.
Overall, individuals who experience disability are at greater risk for being hospitalized either because they have contracted COVID-19 or because pre-existing health conditions have worsened.
Hospital capacity and number of people with disabilities
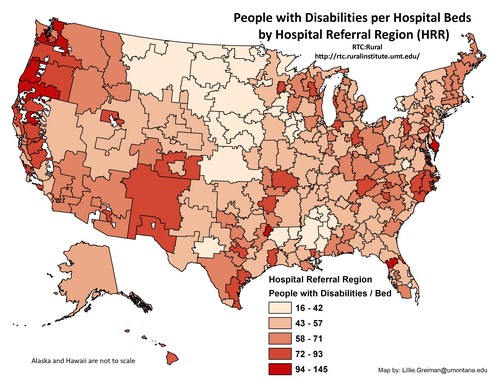
Hospital capacity varies greatly across the nation, as does the prevalence of disability. In order to understand which areas may be most impacted by an influx of patients with disabilities, we analyzed the number of people with disabilities per hospital bed across hospital referral regions. Disability data come from the American Community Survey (2013-2017) and the hospital referral regions were obtained from Harvard Global Health Institute.
Text description: This map outlines hospital referral regions across the United States. Each region is highlighted in shades of red to designate the rate of people with disabilities per hospital bed. Darker shades indicate fewer beds. In general, there are fewer beds available per person in more populated regions such as along the Pacific coast and urban regions in the east. There are also lower rates of bed availability in sparsely populated regions thought the west, such as Nevada, Idaho, Utah, and New Mexico. Regions which include states such as North Dakota, South Dakota, Nebraska, and Kansas appear to have more beds available, while other areas, such as Appalachia and the Southern U.S. are highly variable. Map by: Lillie.Greiman@mso.umt.edu.
Rationing care and equitable access
While limited access to healthcare should be a concern for every citizen, it may be particularly concerning for people with disabilities. Many states have already begun to explore issuing guidance for overburdened hospitals regarding the rationing of care (steps that are already in place in Italy.) For example, the Institute for Health Metrics and Evaluation projects that the state of New York will be short over 10,000 needed intensive care unit beds to treat patients with COVID-19.
Who will get access to a ventilator or an ICU bed when there are not enough for everyone? How will we make these critical decisions?
These theoretical ethical dilemmas are currently playing out in the real world and people with disabilities fear they will be left behind, because historically, they have been. Until recently, people with disabilities were systematically institutionalized and separated from the community precisely because they weren’t considered as “valuable” as able-bodied individuals. This is debatably still the case as people with disabilities are disproportionately represented in prisons and nursing homes.
The current crisis returns us to conversations about who is valuable and who is expendable with terms such as “social usefulness” being openly discussed in news media. The fear being felt by people with disabilities right now is real. While advocates continue to fight for justice, the virus will not wait for the courts.