America at a glance: Early fears realized as COVID-19 surges in rural counties
November 12, 2020
COVID-19 has arrived in rural America. Indeed, the worst outbreaks in October 2020 were in counties with populations less than 50,0001. We knew it was coming2, and yet communities are unprepared to face the significant challenges of caring for COVID-19 patients.
Risks and impacts of COVID-19 are not distributed evenly. This is especially true for people with disabilities and rural residents who face significant challenges to accessing healthcare. For COVID-19, risk increases with advanced age (aged 65 and older), congregate living such as nursing homes and long-term care facilities, and for individuals with several health conditions including asthma, diabetes, blood disorders, serious heart conditions, severe obesity, and for those who are immunocompromised3. Many of these conditions are reported at higher rates among the population of people with disabilities, placing them at higher risk of COVID-19 related complications4.
Rural residents are more likely to report a disability than urban residents5 and experience disability earlier in life6. The risks for rural residents with disabilities are compounded because they face long commutes to specialty and emergency care, closed rural hospital7, lack of transportation infrastructure, few or no ICU beds8, higher rates of chronic health conditions, and higher rates of poverty relative to urban areas2, 9, 10, 11. Additionally, rural residents are less likely to follow public health recommendations for preventing the spread of COVID-1912, 13. This is particularly concerning because rural healthcare systems are already overwhelmed14, 15, 16.
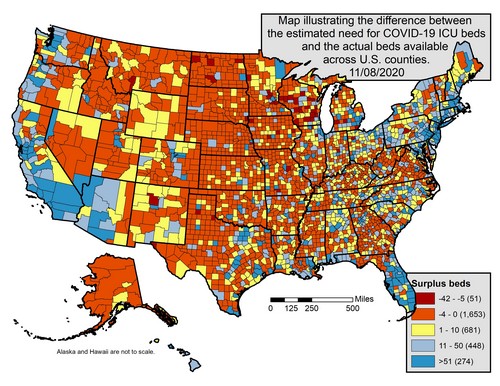
To explore the growing COVID-19 strain on healthcare, we mapped the difference between expected need for ICU beds and local availability. Our map reflects the last week in October through the first week of November, a time period when COVID-19 cases were increasing at steep rates.
Methods
Data for this map come from two sources:
- Active COVID-19 case data for the previous 14 days (October 26th to November 8th) came from the Johns Hopkins Center for Systems Science and Engineering (CSSE) time-series dataset.
- County-level ICU bed capacity data came from the Kaiser Health News Analysis dataset from March, 2020
In addition, we utilized metrics from the CDC’s CovidSurge tool to estimate the number of ICU beds needed based on active Covid-19 cases. This tool estimates that 5.5% of new Covid-19 cases will require hospitalization, and of those, 20% are expected to be admitted to the ICU.
We combined these data to construct a map that represents the difference between ICU bed need and local availability at the county level.
Results
This map shows that many rural counties do not have available ICU beds to meet local need. In particular, large regions in the Midwest, Great Plains, and Mountain West face critical shortages. Across the country we estimate that 1,704 counties do not have enough ICU beds for potential COVID-19 patients. Of these, 1,314 (77%) are rural.
The lack of available beds forces patients to transfer to a larger hospital, in another county for care. This in turn puts pressure on larger regional hospitals that not only provide beds for local populations but also need to meet demand from multiple neighboring counties. For example, nearly half of COVID-19 patients currently being treated in Missoula County, MT are residents from another county17. Additionally, our analysis does not account for the share of ICU beds that will likely be in use or required for non-COVID patients.
Click on the map for a downloadable version.
Text description:
This map shows all counties in the United States classified by the number of surplus ICU beds available after accounting for estimated ICU bed need due to COVID-19 infection. Counties are color classified from dark red, orange, yellow, light blue, dark blue. Red and orange counties, which dominate the map (especially in rural areas in the Midwest, Great Plains and Rocky Mountains) indicate that there are no bed available to meet the need with values ranging from -42 to 0 beds available. Yellow counties have 1-10 beds available, blue counties have 11+ beds available. Urban counties with larger hospital and healthcare infrastructure are more likely to be blue. Fifty one counties are dark red, 1,653 counties are orange, 681 counties are yellow, 448 counties are light blue and 274 counties are dark blue.
Conclusion
The spread of COVID-19 is rampant through rural America. Unfortunately, because CDC projections for ICU needs are based on the general population, they likely underestimate needs from rural communities that have a disproportionate share of those living with disability, advanced age, health complications, and living in congregate settings. These are groups of individuals at increased risk for complications
In addition to bed shortages, staff shortages at local hospitals18 are also adding strain to overextended rural healthcare systems. As winter approaches, the worst may not be over, highlighting the need for continued social distancing, mask use, hand washing/sanitizing, and other strategies for limiting the spread of COVID-19.
References
1. Leatherby L. The Worst Virus Outbreaks in the U.S. Are Now in Rural Areas. The New York Times. https://www.nytimes.com/interactive/2020/10/22/us/covid-rural-us.html. Published October 22, 2020.
2. Monnat SM. Why Coronavirus could hit rural areas harder. Lerner Center for Public Health Promotion. 2020;(16):5.
3. CDC. Coronavirus Disease 2019 (COVID-19): People who need to take extra precautions. Centers for Disease Control and Prevention. Published July 21, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html
4. CDC. Disability and Health Related Conditions. Centers for Disease Control and Prevention. Published September 9, 2019. https://www.cdc.gov/ncbddd/disabilityandhealth/relatedconditions.html
5. von Reichert C, Greiman L, Myers A, Rural Institute U of M. The Geography of Disability in America: On Rural-Urban Differences in Impairment Rates. Independent Living and Community Participation. 2014;7. https://scholarworks.umt.edu/ruralinst_independent_living_community_participation/7
6. Sage R, Ward B, Myers A, Ravesloot C. Transitory and Enduring Disability Among Urban and Rural People. The Journal of Rural Health. 2018;0:1-11. doi:10.1111/jrh.12338
7. Tribble SJ. Prognosis for Rural Hospitals Worsens With Pandemic. Kaiser Health News. Published August 26, 2020. https://khn.org/news/rural-hospital-closures-worsen-with-pandemic/
8. Millions Of Older Americans Live In Counties With No ICU Beds As Pandemic Intensifies | Kaiser Health News. https://khn.org/news/as-coronavirus-spreads-widely-millions-of-older-americans-live-in-counties-with-no-icu-beds/
9. CSELS, OPHHS, CDC. About Rural Health. Published August 2, 2017. https://www.cdc.gov/ruralhealth/about.html
10. Gamm L, Hutchison L, Bellamy G, Dabney BJ. Rural Healthy People 2010: Identifying rural health priorities and models for practice. The Journal of Rural Health. 2002;18(1):9-14. doi:10.1111/j.1748-0361.2002.tb00869.x
11. NIHCM – Rural Health in America: How Shifting Populations Leave People Behind. https://www.nihcm.org/categories/rural-health-in-america-how-shifting-populations-leave-people-behind
12. Siegler K. Why Parts Of Rural America Are Pushing Back On Coronavirus Restrictions. NPR.org. Published March 27, 2020. https://www.npr.org/2020/05/27/862831144/why-parts-of-rural-america-are-pushing-back-on-coronavirus-restrictions
13. Myers A., Ipsen, C., Smith, L., and the Research and Training Center on Disability in Rural Communities. (July 2020). America at a glance: COVID-19 and disability in rural areas. Missoula, MT: The University of Montana, Rural Institute for Inclusive Communities
14. COVID-19 Surges In Rural Communities, Overwhelming Some Local Hospitals. NPR.org. Accessed November 2, 2020. https://www.npr.org/sections/health-shots/2020/10/22/926264615/covid-19-surges-in-rural-communities-overwhelming-some-local-hospitals
15. ‘We are broken’: Montana health care workers battle growing Covid outbreak. NBC News. Accessed November 2, 2020. https://www.nbcnews.com/news/us-news/we-are-broken-montana-health-care-workers-battle-growing-covid-n1245526
16. Rural U.S. Hospitals Are on Life Support as a Third Wave of COVID-19 Strikes. Time. Accessed November 2, 2020. https://time.com/5901656/coronavirus-hospital-closures/
17. Missoula County: Record 106 COVID-19 cases Saturday. Missoulian. Accessed November 9, 2020. https://missoulian.com/news/local/missoula-county-record-121-covid-19-cases-saturday/article_8119a7e3-9e58-5b1c-bebd-1cf9bfe60045.html
18. Hi-Line hospitals see shortage of health care workers amid COVID-19 surge. Missoulian. Accessed November 9, 2020. https://missoulian.com/news/state-and-regional/hi-line-hospitals-see-shortage-of-health-care-workers-amid-covid-19-surge/article_4bf44d41-b028-5e06-a42f-26e9e4ef73b0.html#tracking-source=home-the-latest